The structure and functioning of the urinary system is very complex. I will therefore try to explain in a simple but logical way everything that happens around the excretory system and urination, so that you can later understand the reasons for all these recommendations and, with empowerment, make changes in your life that will lead you to suffer less often from uncomfortable cystitis or other more serious urinary conditions.
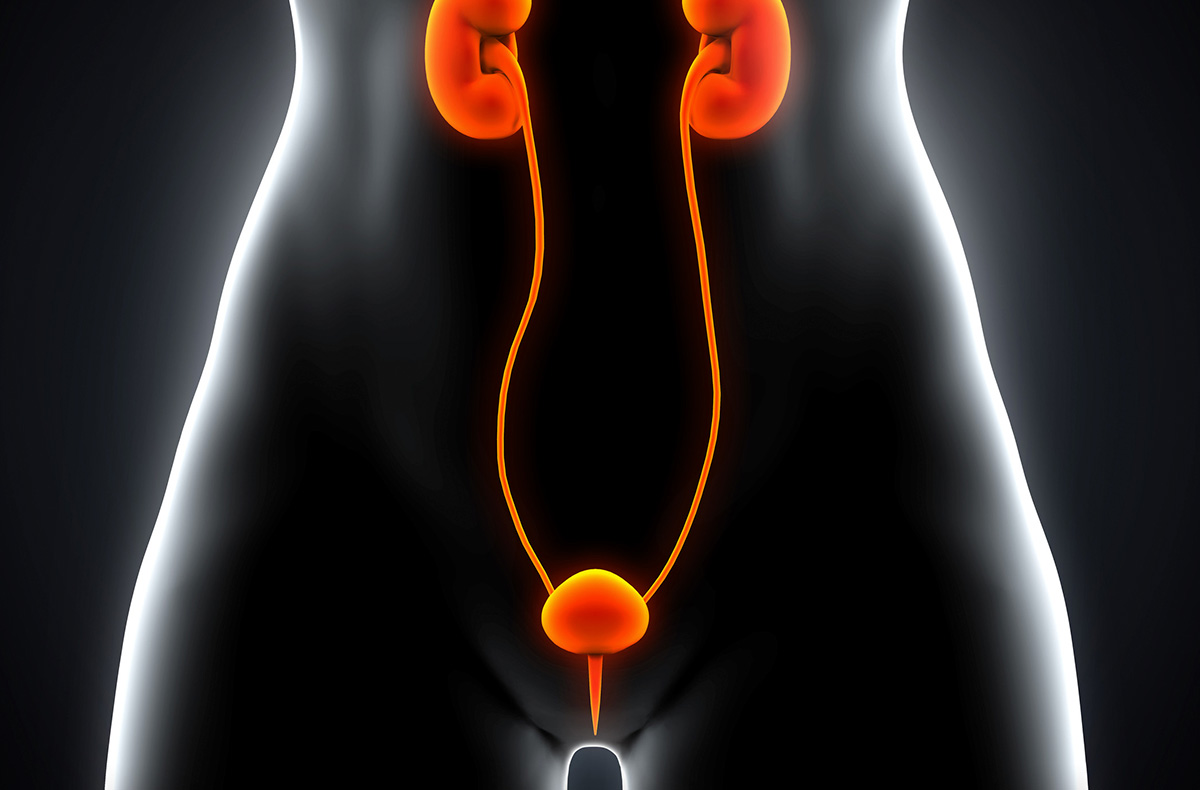
The urinary system consists of the kidneys, which are the urine-producing organs, on the one hand, and the pyelocaliceal system, the ureters, the urinary bladder and the urethra, which are the urine excretory organs, on the other. The vast majority of urological diseases are based in the excretory system. Therefore, I will focus on this system to give a brief summary of the anatomy and physiology (how it functions under normal conditions), without dealing with the complex structure of the interior of the kidney, which is of little relevance to the topic at hand.
The urinary excretory system is made up of several layers of tissue. From the inside to the outside, and speaking in a very simplified way, we find the mucosa, which is the inner lining of the renal pelvis, ureters, bladder and urethra. Its function is to act as an impermeable barrier to the passage of urine. The cells lining this mucosa, called urothelial cells, have the particularity of having a series of proteins on their surface, the uroplakins, whose function, among others, is to protect the excretory system from infection. However, some germs, such as the bacterium
Escherichia coli The mucosa of the urothelial cells, a common cause of urinary tract infections, has "hairs" called fimbriae on its surface that allow it to attach to precisely these receptors (especially uroplakin Ia) and even penetrate into the urothelial cells. The mucosa is also covered by a layer of mucus, mainly made up of complex sugars called glycosaminoglycans (GAGs), including hyaluronic acid and chondroitin sulphate, which protect it from physical, chemical or biological aggression and make it impermeable.
Under the mucosa, and separated from it by a thin layer called the basement membrane, on which the urothelial cells rest, we find the lamina propria, a tissue made up of different types of fibres (collagen, elastic fibres, etc.), blood and lymphatic vessels, nerve endings, some support cells such as fibroblasts, myofibroblasts or adipocytes (fat cells), and immune cells.
The function of the submucosa is to give structural support to the mucosa, as well as to provide immune defence if necessary, reinforcing the defence capacity that already exists in the urothelium. The resident immune system of the bladder consists mainly of cells of innate immunity (non-specialised cells, with no "immunological memory"), mainly mast cells and macrophages, as well as some natural killer (Nk) cells. These cells, together with secretory immunoglobulin A (the antibodies that usually reside in the mucosa), uroplakins, the mucus layer and some bactericidal substances secreted into the urine from certain renal or bladder cells (Tamm-Horsfall protein, β-defensin 1, NGAL, ribonuclease 7, cathelicidin, pentraxins, etc.), form the first line of defence against infection. If the innate immune response is activated by an infection, cytokines will be released by both immune cells and urothelial cells, which are substances that serve to "call for reinforcements", recruiting other immune cells to help reinforce the innate immune response (neutrophils, more macrophages, lymphocytes, etc.).
After the lamina propria, we find the muscularis propria, a layer of muscle fibres arranged in different directions that allow movements to be created in these organs, so that urine can move from the kidneys to the bladder and then be expelled by the bladder during urination. In the bladder, this muscle is called the detrusor muscle. Its function is controlled by the autonomic nervous system (sympathetic and parasympathetic systems), which we will discuss in more detail in another article. The muscular layer, together with the submucosal layer and its elastic fibres, gives the bladder a large capacity to store about half a litre of urine, without the pressure inside it increasing at rest. This mechanism is very important for the proper functioning of the entire urinary system, as overpressure in the bladder could be transmitted retrograde to the kidneys, leading to kidney dysfunction, as the kidneys always need to work at low pressure. Also, during urination, when the bladder muscle contracts to expel urine and the pressure increases greatly, the special arrangement of smooth muscle fibres at the mouth of the ureters works as if it were a valve, preventing this pressure from being transmitted to the kidneys. If this closure mechanism does not occur properly, a pathological situation known as "vesico-ureteral reflux" occurs. On the other hand, mention should be made of the sphincteric mechanism of the bladder and urethra, i.e. the muscles that "close" the end of the excretory system and prevent urine from constantly escaping to the outside. We can consider that there are two sphincters in the bladder, the internal sphincter or bladder neck and the external sphincter or striated sphincter. The internal sphincter is nothing more than the extension of the muscle fibres of the bladder wall, which become circular at the transition point between the bladder and the urethra. Thus, when they contract, they close the bladder outlet, while when they open, the bladder takes the shape of a funnel and urine can pass through. The external sphincter is not strictly speaking part of the urinary excretory system, but it is closely linked to it. It is a circular muscle that surrounds the middle urethra in women, and the membranous urethra in men (the part of the urethra just below the prostate). This muscle is part of a muscle group called the "pelvic floor", whose function is to give anatomical and functional support to the pelvic organs. Contraction of the external sphincter allows the urethra to be "strangulated" to prevent urine from passing. In this way, together with the help of the internal sphincter, correct continence is achieved. Unlike the bladder neck, whose function is governed by the autonomic nervous system, and which we cannot control voluntarily, the external sphincter works by means of fibres from the pudendal nerve, which belongs to the "voluntary" nervous system.
Continuing with the layered structure of the excretory system, we find the outermost layer known as the "serosa", composed mainly of connective tissue. This layer does not cover the entire outer surface of the organs, but provides vascular support for them by supplying numerous blood vessels. In the areas of the excretory system where there is no serosa, there is a layer of loose connective tissue called the adventitia, which has the same function.
Bibliography:
Arponen S (2021). Es la microbiota, idiota. Alienta.
Godaly G, Ambite I, Svanborg C. Innate immunity and genetic determinants of urinary tract infection susceptibility. Curr Opin Infect Dis. 2015 Feb;28(1):88-96.
Lacerda Mariano L, Ingersoll MA. Bladder resident macrophages: Mucosal sentinels. Cell Immunol. 2018 Aug;330:136-141.
Song J, Abraham SN. TLR-mediated immune responses in the urinary tract. Curr Opin Microbiol. 2008 Feb;11(1):66-73.
Becknell B, Ching C, Spencer JD. The Responses of the Ribonuclease A Superfamily to Urinary Tract Infection. Front Immunol. 2019 Nov 29;10:2786.
Steigedal M, Marstad A, Haug M, Damås JK, Strong RK, et al. Lipocalin 2 imparts selective pressure on bacterial growth in the bladder and is elevated in women with urinary tract infection. J Immunol. 2014 Dec 15;193(12):6081-9.
Ueda N, Kondo M, Takezawa K, Kiuchi H, Sekii Y, et al. Bladder urothelium converts bacterial lipopolysaccharide information into neural signaling via an ATP-mediated pathway to enhance the micturition reflex for rapid defense. Sci Rep. 2020 Dec 3;10(1):21167.
Hayes BW, Abraham SN. Innate Immune Responses to Bladder Infection. Microbiol Spectr. 2016 Dec;4(6):10.1128/microbiolspec.UTI-0024-2016.
O’Brien VP, Hannan TJ, Schaeffer AJ, Hultgren SJ. Are you experienced? Understanding bladder innate immunity in the context of recurrent urinary tract infection. Curr Opin Infect Dis. 2015 Feb;28(1):97-105.
Huang J, Fu L, Huang J, Zhao J, Zhang X, et al. Group 3 Innate Lymphoid Cells Protect the Host from the Uropathogenic Escherichia coli Infection in the Bladder. Adv Sci (Weinh). 2022 Feb;9(6):e2103303.
Wu J, Abraham SN. The Roles of T cells in Bladder Pathologies. Trends Immunol. 2021 Mar;42(3):248-260.
Billips BK, Schaeffer AJ, Klumpp DJ. Molecular basis of uropathogenic Escherichia coli evasion of the innate immune response in the bladder. Infect Immun. 2008 Sep;76(9):3891-900.
Nielsen KL, Stegger M, Kiil K, Godfrey PA, Feldgarden M, Lilje B, Andersen PS, Frimodt-Møller N. Whole-genome comparison of urinary pathogenic Escherichia coli and faecal isolates of UTI patients and healthy controls. Int J Med Microbiol. 2017 Dec;307(8):497-507.
Ambite I, Butler D, Wan MLY, Rosenblad T, Tran TH, Chao SM, Svanborg C. Molecular determinants of disease severity in urinary tract infection. Nat Rev Urol. 2021 Aug;18(8):468-486.
Ziegler T, Jacobsohn N, Fünfstück R. Correlation between blood group phenotype and virulence properties of Escherichia coli in patients with chronic urinary tract infection. Int J Antimicrob Agents. 2004 Sep;24 Suppl 1:S70-5.
Sulaiman KA, Al Qahtani N, Al Muqrin M, Al Dossari M, Al Wabel A, et al. The correlation between non-O blood group type and recurrent catheter-associated urinary tract infections in critically ill patients: A retrospective study. J Int Med Res. 2022 Jul;50(7):3000605221108082.
Albracht CD, Hreha TN, Hunstad DA. Sex effects in pyelonephritis. Pediatr Nephrol. 2021 Mar;36(3):507-515.
Wnorowska U, Piktel E, Deptuła P, Wollny T, Król G, et al. Ceragenin CSA-13 displays high antibacterial efficiency in a mouse model of urinary tract infection. Sci Rep. 2022 Nov 10;12(1):19164.