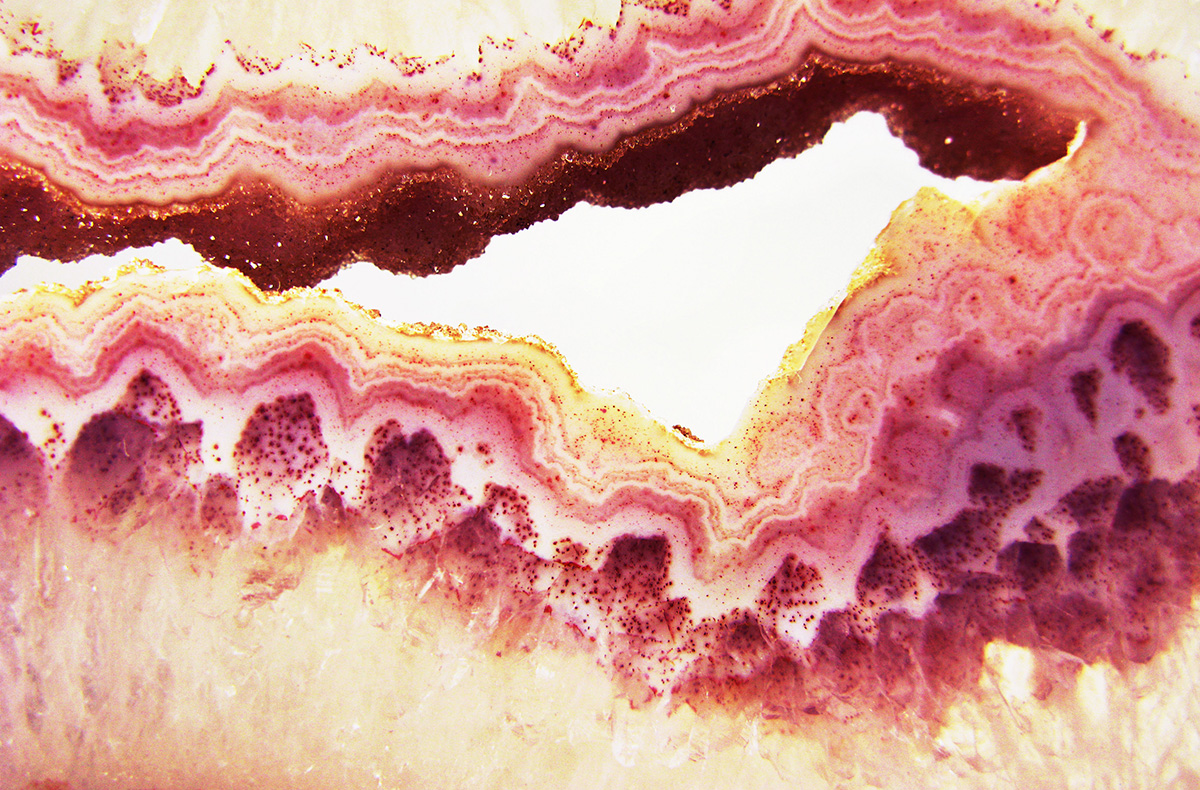
The intestinal wall is made up of several layers of specialised tissues and cells whose arrangement in the form of small folds called intestinal villi allows it to facilitate digestion and absorption of nutrients. From the inside to the outside we find the mucosa, the submucosa, the muscular layer and the outermost serosa. The epithelium of the intestinal mucosa consists of a single layer of cells. It is lined with mucus, a substance that gives it protection and allows it to harbour numerous bacteria of the intestinal microbiota. The most numerous cells are the enterocytes, tall, narrow cells, which are responsible for the absorption of nutrients. The surface of the enterocytes that is in contact with the intestinal lumen and mucus is not smooth, but forms small protrusions called microvilli, which greatly increase the surface area for nutrient absorption. This is also known as the "brush border". In addition, these microvilli contain certain digestive enzymes such as lactase (which allows us to digest the lactose in milk), maltase (which digests maltose), sucrase (which digests sucrose) or aminopeptidase (which digests small proteins called di- or tripeptides and amino acids). Among the enterocytes are goblet cells, which are responsible for producing and secreting mucus. There are also endocrine cells, which release hormones such as secretin and cholecystokinin, which control the secretion of digestive enzymes by the pancreas and gallbladder. In the intestinal crypts, the deepest part of the villi, stem cells are located, which divide and differentiate as the surface cells die. These cells are responsible for the renewal and regeneration of the intestinal epithelium. Beneath the mucosa is the submucosa, which is made up of connective tissue and blood capillaries, and is responsible for supplying nutrients and oxygen to the cells of the intestine, and also for collecting and transporting the products of digestion through the bloodstream. The next layer is the muscle layer, which is divided into two sub-layers: the inner circular and the outer longitudinal. These layers are made up of smooth muscle cells, whose movement is governed by the nerves of the enteric nervous system (related to the sympathetic and parasympathetic autonomic nervous system) and are responsible for the movements of the intestine. These movements, such as peristalsis, segmentation, the migratory motor complex, colonic motility or reflexes, are what allow us to digest properly, as well as transport food along the gastrointestinal tract and eliminate it in the faeces. The outermost layer of the intestinal wall is the serosa, which is composed of connective tissue and epithelial cells. It contains blood vessels and is responsible for protecting and supporting the intestine.
The gut has its own nervous system, known as the "enteric nervous system". It is made up of about 80 to 100 million neurons, as many as there are in the spinal cord. It has the capacity to function independently, but is also connected to the central nervous system via the autonomic (sympathetic and parasympathetic) nervous system. It has two main components, Meissner's submucosal plexus, located below the submucosa, and Auerbach's myenteric plexus, located between the circular and longitudinal muscle layers. Meissner's plexus is most developed in the small intestine and colon.
It is primarily concerned with regulating digestion and absorption at the level of the mucosa and blood vessels, depending on the stimulation produced by nutrients. Auerbach's plexus coordinates the activity of the muscle layers to enable the bowel movements I mentioned earlier.
– Leaky - gut" or Porous Intestine
The intestinal wall has a complex structure. It is lined by a single layer of rectangular cells called enterocytes. These cells are bound together by proteins called "tight junctions" on their side walls and are impermeable to the passage of substances, unless the enterocytes "authorise" their opening. Thus, most of the substances we absorb pass through these cells to enter our body, rather than between them, allowing better control of what does and does not pass through. These cells also have a 'brush border' at the top (the part that faces the intestinal lumen), which are tiny hairs called microvilli that allow them to absorb many substances very efficiently. Also, on the surface of the microvilli are certain enzymes that help to finish digesting food, the digestion of which began in the lumen of the stomach or intestine thanks to gastric or pancreatic juices, which are liquids loaded with digestive enzymes that are released when we eat. An example of this is lactose, the sugar contained in dairy products, which is digested at the level of the intestinal microvilli thanks to an enzyme called lactase, and whose deficiency can lead to the famous lactose intolerance. When there is chronic inflammation in the intestinal wall, enterocytes can die or lose their microvilli, and this can lead to malabsorption, poor digestion or even intolerance (for example, lactose intolerance can be genetic if the gene encoding lactase is missing, or it can be acquired through excessive chronic intestinal inflammation). Also, "pores" can open up between cells due to loss or malfunction of tight junctions, so that the tightness of these junctions is lost. There are also molecules such as gluten gliadin (the non-water-soluble part of gluten) that have the ability to bind directly to the tight junctions and open them. Thus, even in the absence of inflammation, these foods can produce intestinal porosity "per se". Intestinal porosity allows substances that should normally remain in the intestinal lumen and not enter our body, such as toxins or pieces of the wall of some intestinal bacteria called lipopolysaccharides, to pass the intestinal barrier without any control by enterocytes. Thus, these substances directly provoke a local inflammatory reaction or even pass into the bloodstream causing inflammation at a distance. For example, lipopolysaccharides can cross the blood-brain barrier, reach the brain and cause neuroinflammation (inflammation of the central nervous system). This is thought to be one of the mechanisms favouring the onset of neurodevelopmental disorders in children, such as autism for example, or neurodegenerative diseases such as Parkinson's or Alzheimer's in adults.
Bibliography:
Arponen S (2021). Es la microbiota, idiota. Alienta.
Godaly G, Ambite I, Svanborg C. Innate immunity and genetic determinants of urinary tract infection susceptibility. Curr Opin Infect Dis. 2015 Feb;28(1):88-96.
Lacerda Mariano L, Ingersoll MA. Bladder resident macrophages: Mucosal sentinels. Cell Immunol. 2018 Aug;330:136-141.
Song J, Abraham SN. TLR-mediated immune responses in the urinary tract. Curr Opin Microbiol. 2008 Feb;11(1):66-73.
Becknell B, Ching C, Spencer JD. The Responses of the Ribonuclease A Superfamily to Urinary Tract Infection. Front Immunol. 2019 Nov 29;10:2786.
Steigedal M, Marstad A, Haug M, Damås JK, Strong RK, et al. Lipocalin 2 imparts selective pressure on bacterial growth in the bladder and is elevated in women with urinary tract infection. J Immunol. 2014 Dec 15;193(12):6081-9.
Ueda N, Kondo M, Takezawa K, Kiuchi H, Sekii Y, et al. Bladder urothelium converts bacterial lipopolysaccharide information into neural signaling via an ATP-mediated pathway to enhance the micturition reflex for rapid defense. Sci Rep. 2020 Dec 3;10(1):21167.
Hayes BW, Abraham SN. Innate Immune Responses to Bladder Infection. Microbiol Spectr. 2016 Dec;4(6):10.1128/microbiolspec.UTI-0024-2016.
O’Brien VP, Hannan TJ, Schaeffer AJ, Hultgren SJ. Are you experienced? Understanding bladder innate immunity in the context of recurrent urinary tract infection. Curr Opin Infect Dis. 2015 Feb;28(1):97-105.
Huang J, Fu L, Huang J, Zhao J, Zhang X, et al. Group 3 Innate Lymphoid Cells Protect the Host from the Uropathogenic Escherichia coli Infection in the Bladder. Adv Sci (Weinh). 2022 Feb;9(6):e2103303.
Wu J, Abraham SN. The Roles of T cells in Bladder Pathologies. Trends Immunol. 2021 Mar;42(3):248-260.
Billips BK, Schaeffer AJ, Klumpp DJ. Molecular basis of uropathogenic Escherichia coli evasion of the innate immune response in the bladder. Infect Immun. 2008 Sep;76(9):3891-900.
Nielsen KL, Stegger M, Kiil K, Godfrey PA, Feldgarden M, Lilje B, Andersen PS, Frimodt-Møller N. Whole-genome comparison of urinary pathogenic Escherichia coli and faecal isolates of UTI patients and healthy controls. Int J Med Microbiol. 2017 Dec;307(8):497-507.
Ambite I, Butler D, Wan MLY, Rosenblad T, Tran TH, Chao SM, Svanborg C. Molecular determinants of disease severity in urinary tract infection. Nat Rev Urol. 2021 Aug;18(8):468-486.
Ziegler T, Jacobsohn N, Fünfstück R. Correlation between blood group phenotype and virulence properties of Escherichia coli in patients with chronic urinary tract infection. Int J Antimicrob Agents. 2004 Sep;24 Suppl 1:S70-5.
Sulaiman KA, Al Qahtani N, Al Muqrin M, Al Dossari M, Al Wabel A, et al. The correlation between non-O blood group type and recurrent catheter-associated urinary tract infections in critically ill patients: A retrospective study. J Int Med Res. 2022 Jul;50(7):3000605221108082.
Albracht CD, Hreha TN, Hunstad DA. Sex effects in pyelonephritis. Pediatr Nephrol. 2021 Mar;36(3):507-515.
Wnorowska U, Piktel E, Deptuła P, Wollny T, Król G, et al. Ceragenin CSA-13 displays high antibacterial efficiency in a mouse model of urinary tract infection. Sci Rep. 2022 Nov 10;12(1):19164.